Ear Surgery (Otoplasty)
Consultations offered at our three convenient locations in Encino, Glendale and Bakersfield
Adults and children alike are often unhappy with the appearance of their ears. If the size, shape, or protrusion of your ears is problematic for you, ear surgery could be the answer you are looking for.
Ear surgery, also called otoplasty, is used to permanently correct any issue you may have with your ears. These procedures are often also referred to as ear pinning or ear reduction surgery. Because they are cosmetic surgical procedures, however, they can only treat the appearance of the external ear.
Otoplasty is performed using an incision in the back of the ear. Special sutures are then placed within the structure of the outer ear to pin it closer to the head. The cartilage may also be removed to reshape the ear if it is too large or comes to a point, or simply repositioned. Ear surgery can also be used in cases of traumatic injury or excessive stretching with large-gauge earrings to reshape the ears into a more natural shape.
Ear surgery is the most popular plastic surgery among children. In fact, it is often recommended that kids get this surgery as soon as possible. There are two reasons for this. First, ears reach adult size around age seven in most people, at which point they can be operated on safely. The other reason that most people choose to do this procedure as early as possible is to spare the child from the teasing that often comes with having big ears.
Dr. Younai has performed countless ear surgeries and can make your ears aesthetically pleasing, no matter what your current issue is. Following surgery, your results should be immediately apparent. You will need to avoid strenuous or potentially dangerous activities during your recovery, and will be asked to sleep with your head elevated for a few days following surgery. You scars will be naturally concealed in the folds behind your ears, and the results are permanent.
Contents
- 1 Introduction
- 2 Before and After Photos
- 3 Surgical Techniques
- 4 Candidates
- 5 Preparation
- 6 Recovery
- 7 Post-surgery Care
- 8 Risks and Complications
- 8.1 Bleeding
- 8.2 Infection
- 8.3 Change in Skin Sensation
- 8.4 Ear Trauma
- 8.5 Skin Contour Irregularities
- 8.6 Scarring
- 8.7 Surgical Anesthesia
- 8.8 Asymmetry
- 8.9 Delayed Healing
- 8.10 Allergic Reactions
- 8.11 Shock
- 8.12 Pain
- 8.13 Damage to Deeper Structures
- 8.14 Sutures
- 8.15 Skin Discoloration / Swelling
- 8.16 Skin Sensitivity
- 8.17 Cardiac and Pulmonary Complications
- 9 Additional Advisories
- 10 Additional Surgery
Introduction
Otoplasty, also known as Ear Pinning, Ear Pinback, or Ear Reduction Surgery, is the cosmetic plastic surgery procedure that permanently corrects protruding ears.
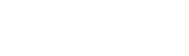
Otoplasty does so by positioning the ears closer to the head (Ear Pinning), reshaping them, reducing their size, and making them more symmetrical. Protruding Ear Deformity is the most prevalent congenital malformation of the head and neck area.
Besides Protruding Ears, other External Ear deformities are also corrected by Otoplasty. These deformities include: Cup Ear or irregular development of the outer ears; Lop Ear or Bat Ear, where the edge of the ear’s exterior grows at a sharp and protruding angle; Cauliflower Ear, caused by crush injury to ear cartilage; “Spock’s Ear” with protruding sharp edge; Shell Ear, with missing folds and creases, as well as ears that are too large or too small.
Otoplasty ranks as the most commonly performed plastic surgery Procedure on children between ages five and fourteen.
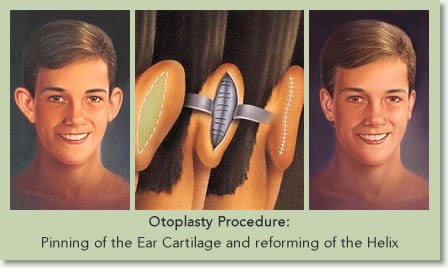
Ear Pinning is one cosmetic surgery where “earlier is better” because of the devastating blows to a child’s self-esteem, who is teased for having protruding ears; being called names such as “Dumbo,” “Mickey Mouse” and “Rabbit Ears.” The optimal time for performing otoplasty in children is just before they start school, or at about the age of seven. At this age the ears have grown to nearly their adult size and the child is old enough to be able to undergo surgery safely. It also gives children a chance to correct their facial deformity before starting to socialize with peers in school.
Otoplasty has also been a blessing for thousands of adults who have spent their lives feeling self-conscious about their “big ears.” They have hidden their ears with hairstyles, hats, and avoided wearing ear jewelry. With Otoplasty they have gained the freedom to wear their hair short or pulled back, wear earrings, and no longer feel embarrassed about their look. While Otoplasty aims to normalize the appearance of the ears it can never produce perfect and fully symmetrical ears. Therefore, parents who are considering Ear Pinning for their children, and adults who are considering the procedure, should have realistic expectations. After all, no two ears are ever identical or perfectly symmetrical.
 Contraindications for Otoplasty include active ear infection. Children who need to undergo surgery on their ear drums, mastoids, or tonsils should delay having Otoplasty.
Contraindications for Otoplasty include active ear infection. Children who need to undergo surgery on their ear drums, mastoids, or tonsils should delay having Otoplasty.
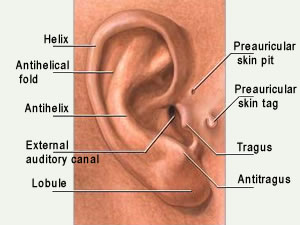
Otoplasty is tailored by plastic surgeons according to the patient’s needs. Techniques include rearranging or sculpting existing ear cartilage; adjusting the position of the ear helix and lobe to that of the head; rearranging, excising or adding skin or cartilage grafts and flaps.
Children having Otoplasty will undergo general anesthesia to assure that they will remain still for maximum safety. On the other hand, adults can undergo Ear Pinning with local anesthesia and sedation, if they have a calm nature.
The Cosmetic plastic surgeon begins the surgery by making an incision just behind the ear, in the natural fold where the ear joins the head. He or she may employ Cartilage Cutting or Cartilage Sparing techniques. Cartilage Sparing, which repositions the cartilage via multiple suspension sutures rather than cutting, has the advantage of avoiding visible edges of cut cartilage, but is technically more challenging. Following the repositioning of the cartilage, the plastic surgeon will address the protrusion of the ear lobes, remove excess skin and close the wound with sutures.
Your Plastic Surgeon’s instructions for recovery will include wearing a special headband or bandage to hold the ears in place, avoid strenuous sports for a period of time, and to sleep with your head elevated for a few days. Following all instructions will be crucial to an optimal outcome.
Before and After Photos
Surgical Techniques
Timing
Otoplasty is one of the few cosmetic surgeries commonly performed on children. It is a case where “earlier is better” because of the devastating psychological impact of peer ridicule.
By age five or six, the “auricle,” the visible, cartilaginous part of the ear, has nearly reached its adult-sized and can be safely corrected. (Only the ear lobes continue to elongate which gives the impression that the ears are still growing). While all surgery carries risk, Otoplasty is overwhelmingly safe and successful. Having it done at a young age is desirable because the cartilage is still very pliable, giving the plastic surgeon more latitude for shaping, and because of the psychological benefit to the child who has the cosmetic improvement prior to starting his or her schooling.
 Parents are advised to monitor their children’s feelings before seriously considering Otoplasty. Parents should not insist on the surgery unless their child wants the change, so that he or she will be more cooperative during the process and be happy with the outcome.
Parents are advised to monitor their children’s feelings before seriously considering Otoplasty. Parents should not insist on the surgery unless their child wants the change, so that he or she will be more cooperative during the process and be happy with the outcome.
Ear pinning is also commonly performed in adults, many of whom have spent years self-consciously hiding their ears with hairstyles and hats. One challenge for older patients is that their cartilage is firmer than that of a child, and more difficult to mold.
Methods
Otoplasty, the reshaping and repositioning of the external ear, is done on an outpatient basis. Performed skillfully, Otoplasty makes the ears more proportional to the size and shape of the head, as well as pinning it back closer to the head. The procedure generally takes about two hours, or one hour per ear, depending upon the degree of correction that his needed.
- Rearranging or sculpting existing cartilage in the ear.
- Adjusting the position of ear helix or ear lobe to the position of the head.
- Rearranging, excising or adding skin.
- Adding cartilage through grafts from elsewhere in the body.
 Before the start of the Otoplasty procedure the patient is either put under sedation or general anesthesia. In young children General Anesthesia is a must, but with adults sedation is an option, as long as they are of calm nature. The ears are further anesthetized with local anesthetics and the ears and scalp are sterilized with antiseptic solution.
Before the start of the Otoplasty procedure the patient is either put under sedation or general anesthesia. In young children General Anesthesia is a must, but with adults sedation is an option, as long as they are of calm nature. The ears are further anesthetized with local anesthetics and the ears and scalp are sterilized with antiseptic solution.
Otoplasty begins with an incision just behind the ear, in the natural fold where the ear is joins the head. The actual techniques involved can be categorized as either Cartilage Splitting (Cutting), or Cartilage Sparing.
Cartilage Cutting involves cutting or weakening of the antihelix, helix or concha. At times a part of the concha is removed in order to reduce its size, thus lessening the auricular prominence and protrusion. The primary disadvantage of this technique is that the edges of cut cartilage can be felt and even sometimes be visualized.
Cartilage Sparing, popularized by Dr. Mustarde, involves reshaping and repositioning the cartilage via multiple suspension sutures placed through the cartilage. The helix and anti-helix folds are created and the ears are literally pinned back! While this technique avoids the possibility of having visible edges of cut cartilage, it is technically more challenging.
Next, the protrusion of the lobules is addressed. The projection and the size of the lobules can both be adjusted by removing excess skin and/or prominent cartilage.
After reshaping and repositioning the ear cartilages, the excess skin folds behind the ears are removed and the wound closed with sutures.
Special ear-protecting bandages are applied and the patient is then awakened from surgery.
It is important to note that even if only one ear needs “pinning back,” surgery will probably be recommended on both ears to achieve the most symmetrical and natural appearance.
Otoplasty may also involve creating a fold in the upper ear in order to fix “shell ears” or “lop ears” in which the folds are not properly formed.
Candidates
 “Did you fly to school or take the bus?” Such cruel taunting is well known to the boys and girls who have the congenital deformity of protruding ears. Called “Dumbo,” “Mickey Mouse”, “rabbit ears,” and any number of other epithets, children who have protruding or deformed ears suffer devastating blows to their self-esteem that can be corrected by Otoplasty.
“Did you fly to school or take the bus?” Such cruel taunting is well known to the boys and girls who have the congenital deformity of protruding ears. Called “Dumbo,” “Mickey Mouse”, “rabbit ears,” and any number of other epithets, children who have protruding or deformed ears suffer devastating blows to their self-esteem that can be corrected by Otoplasty.
Surgery is the only treatment to adequately and permanently correct protruding ears.
Otoplasty can position the ears closer to the head (“ear pinning”), reshape them, reduce their size, and make them more symmetrical. Otoplasty is most commonly performed on children between the ages of five to fourteen. It is one surgery where “earlier is better” in order to prevent the psychological problems that begin when children start their schooling and are subject to continual teasing. Also, ear cartilage is more malleable in a younger patient.
Good Candidates
Otoplasty is a blessing for thousands of adults who have often spent their lives feeling self-conscious about their appearance because of large protruding, deformed or highly asymmetrical ears. They have always hid their large protruding ears under long hair, stayed away from wearing ear-rings, avoided wearing their hair up, and evaded wearing caps.
Protruding ears are genetic, and are the most frequent congenital deformity of the head and neck area – affecting five percent of the general public. Protruding ear deformity affects both genders, and may be unilateral or bilateral. Nearly 60 percent of those affected have a family history of the condition. It is often typified by the failure of the outer rim of the ear to fold back toward the scalp during fetal development. However, there are also deformities caused by trauma (dog or animal bites), or habits of “ear pulling.” Many toddlers pull on their ears during teething stages, and continue to do so even when they are no longer teething. Stretched earlobes can also be corrected by Otoplasty.
Not Good Candidates
“I always wished that I could wear diamond earrings, but was embarrassed by my big ears. After Ear Pin back surgery, I often wear beautiful earrings with my hair up.” — Rachelle, age 40
Because no two ears on any person are identical or completely symmetrical, patients who are considering Otoplasty must realize that Otoplasty will not give them identical ears. Therefore, Otoplasty is contraindicated for those who have unrealistic expectations, as well as those who are not able to comply with the strict postoperative instructions detailed below.
Patients who have previously formed Keloid or Hypertrophic scarring on their ears or other body parts must recognize that they can also have the same outcome with their Otoplasty surgery.
Finally, children who have active ear infections or are to undergo surgery on their ear drums, mastoids, or tonsils should wait until after they have recovered from ear infection or the above-mentioned surgeries before undergoing Otoplasty.
Ear Deformities
- “Cup Ear,” where parts of the outer ear develop irregularly, causing the ear to protrude.
- “Lop Ear” or “Bat Ear“, where the concha (or inner part of the external ear) grows at a right angle of the head instead of parallel to it.
- Large ear lobes.
- “Cauliflower Ear,” a deformity caused by injury and inflammation.
- Deformities of unusual ear shapes, folds and underdevelopment, “Stahl’s Ear Deformity” (satyr, Vulcan or “Spock’s” ear).
- Telephone ear deformity.
- Macrotia (ear too large).
- Microtia (ear too small).
- Shell Ear (curve of the outer rim as well as the folds and creases are missing).
No body parts are perfectly symmetrical. Otoplasty will, however, give the patient’s face a more balanced and symmetrical appearance.
Since the inner ear develops independently, patients with prominent ears generally have normal hearing.
Preparation
“I’ll never forget the day that my son came home crying, with red ears. His classmates were pulling on his ears and teasing him. That was the day that I decided to take him to a plastic surgeon.” — Carol, mother of Jonathan
Preparation for Otoplasty surgery varies depending on whether the patient is a child or adult.
In general, children have to be older than seven years old to undergo otoplasty. Most doctors perform otoplasty for children in the hospital, unless the surgical center is specifically certified to handle children. Children also need a thorough pre-operative evaluation and clearance by their pediatrician. Any person who weighs 100 lbs or more, regardless of age, is considered an adult. The following is the pre-operative instructions for adult patients.
Pre-Operative Checklist

- Approximately one to two weeks before your surgery you will undergo a general pre-operative evaluation at our office, at which time you will also undergo blood testing and EKG if necessary.
- At that time you need to review with our staff all your medical conditions even though they might not appear to be of importance to you. The review of your eye and vision health is also crucial. We would like to know if you had previously undergone any eye or eyelid surgery, do you take any eye drops or medications for your eyes or vision, and do you suffer from dry eye.
- After reviewing the procedure and answering your questions we will give you written instructions of the medications, vitamins, or herbs to avoid for at least two weeks prior and after your surgery. These include over the counter medications or vitamins which might thin your blood and cause you to bleed excessively during and after surgery.
- If you smoke we encourage you to reduce your smoking for one week before and after surgery because this can hamper your healing process.
- You will be provided with prescriptions for pain medications, antibiotics, lubricating eye drops, anti-inflammatory eye drops, and nausea medications. Please have these ready in advance.
- Get your house in order so that after surgery you wouldn’t be bothered with doing demanding house chores.
- Have bags of frozen peas or cold compresses ready in your freezer for use after surgery.
- Have your bed area prepared with many pillows or cushions to be used for propping you up. Elevation of the head after surgery reduces swelling and pain.
- You need to get a soft headband to wear at nights after surgery. This will keep your ears protected during sleep for the next 3 weeks.
- Arrange for adequate support for the care of your children and pets for at least the first two to three days after surgery.
- Have someone reliable, preferably a family member or close friend bring you to surgery and from surgery. This person should be available to stay and assist you the night after surgery. If you don’t have such a person, please let us know in advance so that we can recommend several available after-care facilities or caretakers to you.
- Have loose and comfortable clothes and shoes available to wear the day of surgery. Also if you have dark sunglasses, they will help reduce the sun glare in your eyes after surgery.
- You cannot drink or eat anything except your medications for eight hours prior to surgery.
- Don’t drink any alcohol for one week prior and after your surgery.
- Do not wear any makeup, facial lotions, or perfume the day of surgery. Shower and shampoo the morning of surgery, remove all eyelid and eyebrow cosmetics, and don’t apply any hair gel or grease.
- Bring all your medications with you to surgery.
- Don’t wear jewelry, necklaces, wrist watches, hairpieces, false eyelashes, or contact lenses to surgery.
Before surgery, Dr. Younai and/ or his staff will review with you pre and post operative instructions for Otoplasty, and will furnish you with a written copy of such instructions. Please make sure that you read them in advance. Also, please provide them to whomever who is going to take care of you afterwards.
Recovery
Dos & Don’ts
- Following surgery, the patient’s ears are held in place by a soft elastic bandage or headband which reduces swelling and protects the ears as they heal.
- The ears may feel painful and swollen for a few days, and your plastic surgeon will prescribe pain medication to alleviate the discomfort.
- Also icing over bandages can help reduce swelling and discomfort.
- You are prescribed antibiotics for several days.
- Patients should sleep with their heads elevated the first few nights after surgery in order to minimize swelling. You will be advised to not sleep on your side to avoid placing pressure on your ears.
- After two days, the dressings are removed, after which time you can take a full shower and wet the stitches. If removable, rather than dissolvable stitches are used, they are usually removed within seven to ten days following surgery.

- Once the dressings are removed, you should sleep with a head band which covers your ears and protects them from flopping forward during sleep. At this point you can sleep on a soft pillow in any ways that you choose.
- You can touch your ears gently and apply some Vaseline or vitamin-E ointment in order to help moisturize the skin and to reduce hypersensitivity.
- It is not unusual to feel that your ears are plugged or your sense of hearing is dampened, for several weeks. This is due to the swelling of the ear canal which subsides.
- Children can return to school one to two weeks following surgery. However, the ears will be delicate and need to be protected. The child should avoid physical contact sports for six weeks to avoid damage to the ear.
- Adults can return to work in less than a week, but should also avoid strenuous physical activity for two weeks.
- Both adults and children should wear the “tennis headbands” (no protective helmets) for six weeks during sleep, sports, or in situations when their ears might be hit or traumatized. Afterwards, there is no need for any restrictions.
- If you are planning to have your ears pierced, wait for three weeks.
- Refrain from sun tanning, or at least have your ears covered for four weeks.
- Finally, know that it takes approximately three to five months for the ears to settle, and for the swelling to resolve; so don’t judge them too early.
- Patients are advised to remember that the goal is improvement, not perfection. As is the case with “normal” ears, no two will ever match perfectly, just as no two body parts are perfectly symmetrical.
Post-surgery Care
- Following surgery, the patient’s ears are held in place by a soft elastic bandage or headband which reduces swelling and protects the ears as they heal.
- The ears may feel painful and swollen for a few days, and your plastic surgeon will prescribe pain medication to alleviate the discomfort.
- Also icing over bandages can help reduce swelling and discomfort.
- You are prescribed antibiotics for several days.
- Patients should sleep with their heads elevated the first few nights after surgery in order to minimize swelling. You will be advised to not sleep on your side to avoid placing pressure on your ears.
- After two days, the dressings are removed, after which time you can take a full shower and wet the stitches. If removable, rather than dissolvable stitches are used, they are usually removed within seven to ten days following surgery.
- Once the dressings are removed, you should sleep with a head band which covers your ears and protects them from flopping forward during sleep. At this point you can sleep on a soft pillow in any ways that you choose.
- You can touch your ears gently and apply some Vaseline or vitamin-E ointment in order to help moisturize the skin and to reduce hypersensitivity.
- It is not unusual to feel that your ears are plugged or your sense of hearing is dampened, for several weeks. This is due to the swelling of the ear canal which subsides.
- Children can return to school one to two weeks following surgery. However, the ears will be delicate and need to be protected. The child should avoid physical contact sports for six weeks to avoid damage to the ear.
- Adults can return to work in less than a week, but should also avoid strenuous physical activity for two weeks.
- Both adults and children should wear the “tennis headbands” (no protective helmets) for six weeks during sleep, sports, or in situations when their ears might be hit or traumatized. Afterwards, there is no need for any restrictions.
- If you are planning to have your ears pierced, wait for three weeks.
- Refrain from sun tanning, or at least have your ears covered for four weeks.
- Finally, know that it takes approximately three to five months for the ears to settle, and for the swelling to resolve; so don’t judge them too early.
- Patients are advised to remember that the goal is improvement, not perfection. As is the case with “normal” ears, no two will ever match perfectly, just as no two body parts are perfectly symmetrical.
Risks and Complications
Bleeding
It is possible, though unusual, to experience a bleeding episode during or after surgery. Intraoperative blood transfusions may be required. Should post-operative bleeding occur, it may require an emergency treatment to drain the accumulated blood or blood transfusion. Accumulations of blood under the skin may delay healing and cause scarring. Do not take any aspirin or anti-inflammatory medications for ten days before surgery, as this may increase the risk of bleeding. Non-prescription “herbs” and dietary supplements can increase the risk of surgical bleeding. If blood transfusions are needed to treat blood loss, there is a risk of blood related infections such as hepatitis and the HIV (AIDS). Heparin medications that are used to prevent blood clots in veins can produce bleeding and decreased blood platelets.
Infection
Infection is unusual after surgery. Should an infection occur, additional treatment including antibiotics, hospitalization, or additional surgery may be necessary.
Change in Skin Sensation
It is common to experience diminished (or loss) of skin sensation in areas that have had surgery. Diminished (or complete loss of skin sensation) may not totally resolve after otoplasty surgery.
Ear Trauma
Physical injury after the otoplasty procedure would disrupt the results of surgery. Care must be given to protect the ear(s) from injury during the healing process. Additional surgery may be necessary to correct damage.
Skin Contour Irregularities
Contour irregularities and depressions may occur after otoplasty. Visible and palpable wrinkling of skin and ear cartilage can occur. Residual skin irregularities at the ends of the incisions or “dog ears” are always a possibility and may require additional surgery. This may improve with time, or it can be surgically corrected.
Scarring
All surgery leaves scars, some more visible than others. Although good wound healing after a surgical procedure is expected, abnormal scars may occur within the skin and deeper tissues. Scars may be unattractive and of different color than the surrounding skin tone. Scar appearance may also vary within the same scar. Scars may be asymmetrical (appear different on the right and left side of the body). There is the possibility of visible marks in the skin from sutures used during an otoplasty. In some cases, scars may require surgical revision or treatment.
Surgical Anesthesia
Both local and general anesthesia involves risk. There is the possibility of complications, injury, and even death from all forms of surgical anesthesia or sedation.
Asymmetry
The human face is normally asymmetrical. There can be normal differences between ears in terms of shape and size. There can be a variation from one side to the other in the results obtained from an otoplasty procedure. Additional surgery may be necessary to attempt to revise asymmetry.
Delayed Healing
Wound disruption or delayed wound healing is possible. Some areas of the ear may heal abnormally or may take a long time to heal. Areas of skin may die. This may require frequent dressing changes or further surgery to remove the non-healed tissue. Smokers have a greater risk of skin loss and wound healing complications.
Allergic Reactions
In rare cases, local allergies to tape, suture materials and glues, blood products, topical preparations or injected agents have been reported. Serious systemic reactions including shock (anaphylaxis) may occur to drugs used during surgery and prescription medications. Allergic reactions may require additional treatment.
Shock
In rare circumstances, your surgical procedure can cause severe trauma, particularly when multiple or extensive procedures are performed. Although serious complications are infrequent, infections or excessive fluid loss can lead to severe illness and even death. If surgical shock occurs, hospitalization and additional treatment would be necessary.
Pain
You will experience pain after your surgery. Pain of varying intensity and duration may occur and persist after otoplasty surgery. Chronic pain may occur very infrequently from nerves becoming trapped in scar tissue after an otoplasty.
Damage to Deeper Structures
There is the potential for injury to deeper structures including nerves, blood vessels, muscles, and lungs (pneumothorax) during any surgical procedure. The potential for this to occur varies according to the type of procedure being performed. Injury to deeper structures may be temporary or permanent.
Sutures
Some surgical techniques use deep non-absorbable sutures. You may notice these sutures after your surgery. Sutures may spontaneously poke through the skin, become visible or produce irritation that requires removal.
Skin Discoloration / Swelling
Some bruising and swelling normally occurs following otoplasty. The skin in or near the surgical site can appear either lighter or darker than surrounding skin. Although uncommon, swelling and skin discoloration may persist for long periods of time and, in rare situations, may be permanent.
Skin Sensitivity
Itching, tenderness, or exaggerated responses to hot or cold temperatures may occur after surgery. Usually this resolves during healing, but in rare situations it may be chronic.
Cardiac and Pulmonary Complications
Surgery, especially longer procedures, may be associated with the formation of, or increase in, blood clots in the venous system. Pulmonary complications may occur secondarily to both blood clots (pulmonary emboli), fat deposits (fat emboli) or partial collapse of the lungs after general anesthesia. Pulmonary and fat emboli can be life-threatening or fatal in some circumstances. Air travel, inactivity and other conditions may increase the incidence of blood clots traveling to the lungs causing a major blood clot that may result in death. It is important to discuss with your physician any past history of blood clots or swollen legs that may contribute to this condition. Cardiac complications are a risk with any surgery and anesthesia, even in patients without symptoms. If you experience shortness of breath, chest pains, or unusual heart beats, seek medical attention immediately. Should any of these complications occur, you may require hospitalization and additional treatment.
Additional Advisories
Unsatisfactory Result
Although good results are expected, there is no guarantee or warranty expressed or implied, on the results that may be obtained. You may be disappointed with the results of otoplasty surgery. This would include risks such as asymmetry, unsatisfactory surgical scar location, unacceptable visible deformities at the ends of the incisions (dog ears), loss of facial movement, poor healing, wound disruption, and loss of sensation. It may be necessary to perform additional surgery to improve your results.
Long-Term Results
Subsequent alterations in ear appearance may occur as the result of aging, sun exposure, pregnancy, menopause, or other circumstances not related to otoplasty surgery. Due to the resilient nature of ear cartilage, revisionary surgery may be necessary in order to improve or maintain the results following otoplasty surgery.
Female Patient Information
It is important to inform your plastic surgeon if you use birth control pills, estrogen replacement, or if you believe you may be pregnant. Many medications including antibiotics may neutralize the preventive effect of birth control pills, allowing for conception and pregnancy.
Smoking, Second-Hand Smoke Exposure, Nicotine Products (Patch, Gum, Nasal Spray)
Patients who are currently smoking, use tobacco products, or nicotine products (patch, gum, or nasal spray) are at a greater risk for significant surgical complications of skin dying, delayed healing, and additional scarring. Individuals exposed to second-hand smoke are also at potential risk for similar complications attributable to nicotine exposure. Additionally, smokers may have a significant negative effect on anesthesia and recovery from anesthesia, with coughing and possibly increased bleeding. Individuals who are not exposed to tobacco smoke or nicotine-containing products have a significantly lower risk of this type of complication.
It is important to refrain from smoking at least 6 weeks before surgery and until your physician states it is safe to return, if desired.
Mental Health Disorders and Elective Surgery
It is important that all patients seeking to undergo elective surgery have realistic expectations that focus on improvement rather than perfection. Complications or less than satisfactory results are sometimes unavoidable, may require additional surgery and often are stressful. Please openly discuss with your surgeon, prior to surgery, any history that you may have of significant emotional depression or mental health disorders. Although many individuals may benefit psychologically from the results of elective surgery, effects on mental health cannot be accurately predicted.
Medications
There are many adverse reactions that occur as the result of taking over-the-counter, herbal, and/or prescription medications. Be sure to check with your physician about any drug interactions that may exist with medications which you are already taking. If you have an adverse reaction, stop the drugs immediately and call your plastic surgeon for further instructions. If the reaction is severe, go immediately to the nearest emergency room. When taking the prescribed pain medications after surgery, realize that they can affect your thought process. Do not drive, do not operate complex equipment, do not make any important decisions, and do not drink any alcohol while taking these medications. Be sure to take your prescribed medication only as directed.
Additional Surgery
There are many variable conditions that may influence the long-term result of otoplasty. Secondary surgery may be necessary to obtain optimal results. Should complications occur, additional surgery or other treatments may be necessary. Even though risks and complications occur infrequently, the risks cited are particularly associated with otoplasty surgery. Other complications and risks can occur but are even more uncommon. The practice of medicine and surgery is not an exact science. Although good results are expected, there is no guarantee or warranty expressed or implied, on the results that may be obtained. In some situations, it may not be possible to achieve optimal results with a single surgical procedure.
Patient Compliance
Follow all physician instructions carefully; this is essential for the success of your outcome. It is important that the surgical incisions are not subjected to excessive force, swelling, abrasion, or motion during the time of healing. Personal and vocational activity needs to be restricted. Protective dressings and drains should not be removed unless instructed by your plastic surgeon. Successful post-operative function depends on both surgery and subsequent care. Physical activity that increases your pulse or heart rate may cause bruising, swelling, fluid accumulation and the need for return to surgery. It is wise to refrain from intimate physical activities after surgery until your physician states it is safe. It is important that you participate in follow-up care, return for aftercare, and promote your recovery after surgery.
Health Insurance
Most health insurance companies exclude coverage for cosmetic surgical operations such as otoplasty surgery or any complications that might occur from surgery. Please carefully review your health insurance subscriber information pamphlet. Most insurance plans exclude coverage for secondary or reversionary surgery.
Financial Resonsibiliies
The cost of surgery involves several charges for the services provided. The total includes fees charged by your surgeon, the cost of surgical supplies, anesthesia, laboratory tests, and possible outpatient hospital charges, depending on where the surgery is performed. Depending on whether the cost of surgery is covered by an insurance plan, you will be responsible for necessary co-payments, deductibles, and charges not covered. The fees charged for this procedure do not include any potential future costs for additional procedures that you elect to have or require in order to revise, optimize, or complete your outcome. Additional costs may occur should complications develop from the surgery. Secondary surgery or hospital day-surgery charges involved with revision surgery will also be your responsibility. In signing the consent for this surgery/procedure, you acknowledge that you have been informed about its risk and consequences and accept responsibility for the clinical decisions that were made along with the financial costs of all future treatments.